by Gaurav Dubey (MS Biotechnology)
Today, opioid addiction is a serious global health pandemic that has caused premature disability and death.1,2 With the mortality rate of opioid-dependent persons thirteen times higher than the non-dependent individual, it is clear that this issue has reached epidemic proportions.1 A three-year national longitudinal study in the United States even indicated concerning trends, showing an increase in non-medical opioid use in young adults.3 Identifying effective pharmacologic and behavioral interventions is paramount to quelling this epidemic before the flames spread even further.
Fighting Fire With Fire: Using Opioids to Treat Opioid Addiction
Treating opioid addiction with pharmacologically active opioids to relieve opiate withdrawal symptoms has been a mainstay of opioid-use-disorder drug therapy, and is commonly referred to as Medication Assisted Treatment (MAT).2 This process involves stabilizing the opioid-dependent individual through substitution treatments that attenuate opiate dependence on his or her mental state. Additionally, these treatments provide detoxification (from the user’s drug of choice, not from opioids in general, as patients receiving MAT are still dependent on opioids) to minimize withdrawal symptoms, as well as to provide maintenance in preventing relapse.4,5 Behavioral interventions alone have failed to show good efficacy and have extremely poor outcomes, with over 80% of people returning to drug use.2 Thus, the need for simultaneous pharmacologic intervention is imperative for the successful treatment of opioid addiction.
The 3 Most Common MAT Agents: Methadone, Suboxone & Vivitrol
The two most commonly studied and utilized medications in MAT therapy are methadone and Suboxone (a combination of buprenorphine and nalaxone in a 4:1 ratio). It is critical to note that there does not exist any curative treatments for opioid addiction that are available. However, methadone and Suboxone have shown to effectively reduce withdrawals, diminish cravings, and prevent relapse by blocking the effects of commonly abused opioids. This blog will explore methadone maintenance therapy (MMT), its clinical utility in treating opioid addiction, and various risks that are worth noting when considering this treatment modality.
We will explore buprenorphine pharmacology and efficacy in combating opioid addiction in a future blog. To learn more about Vivitrol and it’s role as an antagonist, check out our evidence-based blog evaluating Vivitrol as a tool to overcome opiate addiction and dependency here.

Methadone Maintenance Therapy (MMT): What Is It?
Methadone is a full-agonist at the µ-opioid receptor that is approved for use by the FDA for the treatment of opioid addiction in 1972.6 It is generally administered in a controlled, clinical setting as a tablet, liquid or dispersible tablet.2 It has been used the longest in the treatment of opioid addiction and, as such, contains the largest body of research supporting its efficacy. Patients receiving methadone maintenance therapy (MMT) must go to their certified clinic for daily dosing until a pre-determined amount of urine screens are passed, indicating abstinence from illicit opioids and other drugs of abuse. This greatly reduces the potential for illicit diversion of methadone, unlike Suboxone, which can be prescribed for self-administration by the patient and will be discussed in a future blog.
Methadone Pharmacology: How Does It Work?
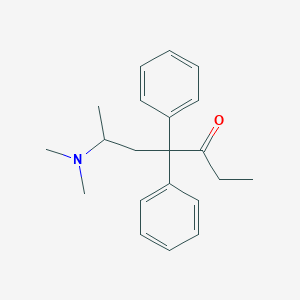
Methadone chemical structure (PubChem)
Methadone is a synthetic opioid that stimulates the µ-opioid receptor as a full-agonist, like other traditional full-agonists such as morphine, hydrocodone, and oxycodone.2 This reduces the euphoric effects of subsequent opioid use and prevents withdrawal following cessation of the opioid being abused.2 It is important to note that while methadone and other traditionally abused opioids (e.g. morphine, heroin, etc…) are full-agonists at the µ -opioid receptor, the significantly longer half-life of methadone that prevents methadone maintenance therapy (MMT) from eliciting the same type of “high” that the more common opioid drugs of abuse provide.
Methadone has a half-life of 24-48 hours, unlike other full-agonist opioid drugs like hydrocodone (Vicodin) and heroin, which have much shorter half-lives (4-6 hours) and provide much greater euphoria. Indeed, studies have demonstrated it is the rapidity with which a drug enters and then exits the brain that is positively correlated with its rewarding and reinforcing effects.8–10 Thus, despite the fact that methadone is also a full-agonist like many opioids of abuse, due to its long half-life, it doesn’t produce the euphoria and compulsion to re-dose like other, more traditional opioids like Vicodin, morphine, heroin, and Fentanyl. Due to this longer half-life, methadone withdrawal is substantially longer than withdrawal from traditional opioids. While clinical literature reports methadone withdrawal to be “milder” in intensity than that of heroin or morphine withdrawal, there is strong anecdotal reporting among MMT patients stating that methadone withdrawal is by far the worst and most torturous of the various opiates. Safe and effective detoxification from methadone should be conducted under the supervision of a physician.
Methadone Pharmacology Continued
Methadone is generally provided as a racemic formulation with the R-entantiomer being responsible for the opioid effect and both R- and S-entantiomers being responsible for its NMDA (N-Methyl D-Aspartate) antagonist action.2 Other drugs that have similar NMDA action are Tramadol, meperdine (Demerol), and dextropropoxyphene. This pharmacologic action on the NMDA receptors has been shown to reduce the buildup of tolerance.2 Methadone is also effective at blocking the effects of other opioids at higher doses (generally at 60mg or above).11
To learn more about basic opioid pharmacology, check out the “Drugs That Act on the Opioid Receptor System Explained” section in this blog.
Methadone Deaths & Risks: What to Watch Out For
“Like other opiate agonists, methadone has the potential to induce lethal respiratory suppression when given in doses that exceed an individual’s tolerance.”2 Indeed, the overdose potential of methadone has long since been an outstanding factor of concern when considering MMT. Nevertheless, methadone safety has been strongly established in the clinical literature, and careful administration by a certified physician is considered safe and effective.12 Since doses as low as 30mg have proven to be fatal in the past, it is advised to induct patients using doses below 30mg and then slowly titrate upward, if needed.13 Combining methadone with benzodiazepines, such as alprazolam (Xanax), has been shown to be especially dangerous, significantly increasing the risk of fatal respiratory depression.13 A similar risk presents itself when combining alcohol with methadone, and patients would be well advised to avoid combining any depressants with methadone, due to its intrinsically potent capacity to induce respiratory depression. This is another key reason methadone patients are required to visit the clinic in person on a daily basis, so staff can accurately assess drug ingestion and clinical status appropriately.
Methadone Side Effects & Adverse Reactions
Methadone is a powerful pharmacologic treatment modality that carries with it several notable side effects that are worth mentioning. Common side effects of methadone include:
- Anxiety
- Restlessness
- Constipation
- Respiratory Depression
- Drowsiness
- Dry Mouth
- Vomiting
- Sexual Dysfunction14
It is imperative to call your healthcare practitioner right away if you experience any of the following symptoms:
- Shallow breathing
- Hallucinations
- Confusion
- Chest Pain
- Dizziness
- Fainting
- Tachycardia (Fast or Pounding Heartbeat)14
As always, it is crucial to inform your healthcare providers of all the medications you are taking—especially since many medications can cause serious adverse interactions if taken together with methadone. Methadone has been shown to cause opioid dependency in the developing fetus if being consumed by a pregnant mother. Patients who are pregnant should consult with their addictionologist and work with their healthcare teams closely to ensure healthy delivery of the baby. It is also important to note that methadone is an addictive drug in its own right, and adequate care should be taken in properly storing and transporting this medication.
Closing Thoughts: Methadone Still Considered “Gold Standard” MAT Therapy
The use of methadone dates back several decades and, as such, troves of clinical data and sound evidence support its use in managing opioid addiction. However, studies have also shown that pharmacologic intervention is not enough to maximize chances for recovery. Behavioral treatments used in conjunction with pharmacotherapy offer the best results for recovering opioid addicts, along with the support of family and friends. If you or someone you know is struggling with opioid addiction or is interested in successfully detoxing off methadone, contact us at ChapelHillDetox.com today!

Image Credit: https://janaburson.wordpress.com/2011/11/25/methadone-dosing-in-opioid-treatment-programs-use-the-evidence/
Works Cited
- Buprenorphine-based regimens and methadone for the medical management of opioid dependence: selecting the appropriate drug for treatment. – PubMed – NCBI. https://www.ncbi.nlm.nih.gov/pubmed/20958853.
- Maintenance Medication for Opiate Addiction: The Foundation of Recovery. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3411273/.
- Boyd, C. J., Teter, C. J., West, B. T., Morales, M. & McCabe, S. E. Non-Medical Use of Prescription Analgesics: A Three-Year National Longitudinal Study. J. Addict. Dis. 28, 232–242 (2009).
- Interested in the latest evidence based information? – BMJ Best Practice. https://bestpractice.bmj.com/info/evidence-information/.
- Gerada, C., National Collaborating Centre for Mental Health (Great Britain), National Institute for Health and Clinical Excellence (Great Britain), British Psychological Society & Royal College of Psychiatrists. Drug misuse: opioid detoxification. (British Psychological Society ; Royal College of Psychiatrists, 2008).
- Pharmacotherapy in the Treatment of Addiction: Methadone. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2885886/.
- Pharmacologic treatments for opioid dependence: detoxification and maintenance options. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3202507/.
- Is methylphenidate like cocaine? Studies on their pharmacokinetics and distribution in the human brain. – PubMed – NCBI. https://www.ncbi.nlm.nih.gov/pubmed/7771915.
- Effects of route of administration on cocaine induced dopamine transporter blockade in the human brain. – PubMed – NCBI. https://www.ncbi.nlm.nih.gov/pubmed/10983846.
- Effects of infusion rate of intravenously administered morphine on physiological, psychomotor, and self-reported measures in humans. – PubMed – NCBI. https://www.ncbi.nlm.nih.gov/pubmed/11714895.
- High-dose methadone produces superior opioid blockade and comparable withdrawal suppression to lower doses in opioid-dependent humans. – PubMed – NCBI. https://www.ncbi.nlm.nih.gov/pubmed/11981600.
- Medical safety and side effects of methadone in tolerant individuals. – PubMed – NCBI. https://www.ncbi.nlm.nih.gov/pubmed/4739193.
- Methadone Deaths: Risk Factors in Pain and Addicted Populations. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2842557/.
- Side Effects of Dolophine (Methadone Tablets), Warnings, Uses. RxList https://www.rxlist.com/methadone-hydrochloride-side-effects-drug-center.htm.
Featured Image Credit: http://www.carf.org/Answering-your-questions-about-methadone/



Recent Comments